Birth Control Methods
Many people who have a uterus and ovaries can potentially become pregnant. People with a penis and testes are potentially capable of getting someone pregnant. For people who are sexually active yet wish to avoid pregnancy, many elements need to be considered when choosing the most appropriate contraceptive method. These elements include safety, effectiveness, availability (including accessibility and affordability), and preference. Voluntary informed choice of contraceptive methods is essential, and contraceptive counseling, when applicable, might be an important contributor to the successful use of contraceptive methods.
In choosing a method of contraception, dual protection from the simultaneous risk for HIV and other STDs also should be considered. Although hormonal contraceptives and IUDs are highly effective at preventing pregnancy, they do not protect against STDs, including HIV (the virus that causes AIDS). Consistent and correct use of latex condoms reduces the risk for HIV infection and other STDs, including chlamydial infection, gonococcal infection, and trichomoniasis.
Ultimately, though, when it comes to heterosexual sex between a partner with a uterus and a partner who produces sperm, the only 100% guaranteed way to avoid pregnancy is abstinence (refraining from sexual activity). For sexually active people of any orientation, wearing condoms may reduce the risk of STDs.
Reversible Methods of Birth Control

Intrauterine Contraception
- Copper T intrauterine device (IUD) —This IUD is a small device that is shaped in the form of a “T.” A doctor places it inside the uterus to prevent pregnancy. It can stay in the uterus for up to 10 years. Typical use failure rate: 0.8%.
- Levonorgestrel intrauterine system (LNG IUD)—The LNG IUD is a small T-shaped device like the Copper T IUD. It is also placed inside the uterus by a doctor. It releases a small amount of progestin each day to prevent pregnancy. The LNG IUD stays in the uterus for up to 5 years. Typical use failure rate: 0.1-0.4%.
Hormonal Methods (for use by people with a uterus and ovaries)

- Implant—The implant is a single, thin rod that is inserted under the skin of the upper arm. The rod contains a progestin that is released into the body over 3 years. Typical use failure rate: 0.01%
- Injection or “shot” (e.g. Depo-provera) —A shot of the hormone progestin in the buttocks or arm every three months. Typical use failure rate: 4%.
- Combined oral contraceptives—Also called “the pill,” combined oral contraceptives contain the hormones estrogen and progestin, and are prescribed by a doctor. A pill is taken at the same time each day. Doctors may advise people older than 35 years who smoke, or have a history of blood clots or breast cancer, to not use the pill. Typical use failure rate: 7%.
- Progestin only pill—Unlike the combined pill, the progestin-only pill (sometimes called the mini-pill) only has one hormone, progestin, instead of both estrogen and progestin, and is prescribed by a doctor. It is taken at the same time each day and may be a good option for people who can’t take estrogen. Typical use failure rate: 7%.
- Patch—This skin patch is worn on the lower abdomen, buttocks, or upper body (but not on the breasts). Prescribed by a doctor, this method releases hormones progestin and estrogen into the bloodstream. A new patch is applied once a week for three weeks. During the fourth week, no patch is worn, to allow for a menstrual period. Typical use failure rate: 7%.
- Hormonal vaginal contraceptive ring—The ring releases progestin and estrogen. You place the ring inside your vagina. You wear the ring for three weeks, take it out for the week you have your period, and then put in a new ring. Typical use failure rate: 7%.
Chemical Methods
- Spermicides—These products work by killing sperm and come in several forms—foam, gel, cream, film, suppository, or tablet. They are placed in the vagina no more than one hour before intercourse. They are then left in place at least six to eight hours after intercourse. A spermicide may be used in addition to a male condom, diaphragm, or cervical cap. They can be purchased at drug stores. Typical use failure rate: 21%.
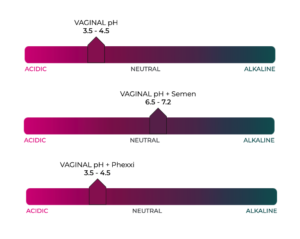
- Phexxi: This on-demand vaginal gel is relatively new, and acts by altering vaginal pH to reduce the motility of sperm, making them unable to swim up the vaginal canal to fertilize an egg. Typical use failure rate: 14% (7% when used as directed).

Barrier Methods
- Diaphragm or cervical cap—These are placed inside the vagina to cover the cervix to block sperm. The diaphragm is shaped like a shallow cup. The cervical cap is a thimble-shaped cup. Before sexual intercourse, one or the other would be inserted, along with spermicide, to block and/or kill sperm. They come in different sizes, so a doctor should be consulted for proper fit. Typical use failure rate for the diaphragm: 17%.
- Sponge—The contraceptive sponge contains spermicide and is placed in the vagina where it fits over the cervix. The sponge works for up to 24 hours and must be left in the vagina for at least 6 hours after the last act of intercourse, at which time it is removed and discarded. Typical use failure rate: 14% for people who have never given birth and 27% for those who have had a baby.

- “Male” condom—Worn on the penis, the condom keeps sperm from getting into the partner’s body. Latex condoms, the most common type, help prevent pregnancy, and HIV and other STDs, as do the newer synthetic condoms. “Natural” or “lambskin” condoms also help prevent pregnancy, but may not provide protection against STDs, including HIV. Typical use failure rate: 13%. Condoms can only be used once. They can be purchased, along with KY jelly, or water-based lubricants, at a drug store. Do not use oil-based lubricants such as massage oils, baby oil, lotions, or petroleum jelly with latex condoms. They will weaken the condom, causing it to tear or break.
- “Female” condom—Worn inside the vagina, this device helps prevent sperm from getting into the body. It is packaged with a lubricant and is available at drug stores. It can be inserted up to eight hours before sexual intercourse. Typical use failure rate: 21%, and also may help prevent STDs. Should not be used in conjunction with a “male” condom, as this could cause one or the other barrier to tear.
- Dental dams – latex or polyurethane sheets used between the mouth and vagina or anus during oral sex. While dental dams do not aid in contraception, they can act as protection against sexually transmitted pathogens.
Fertility Awareness-Based Methods
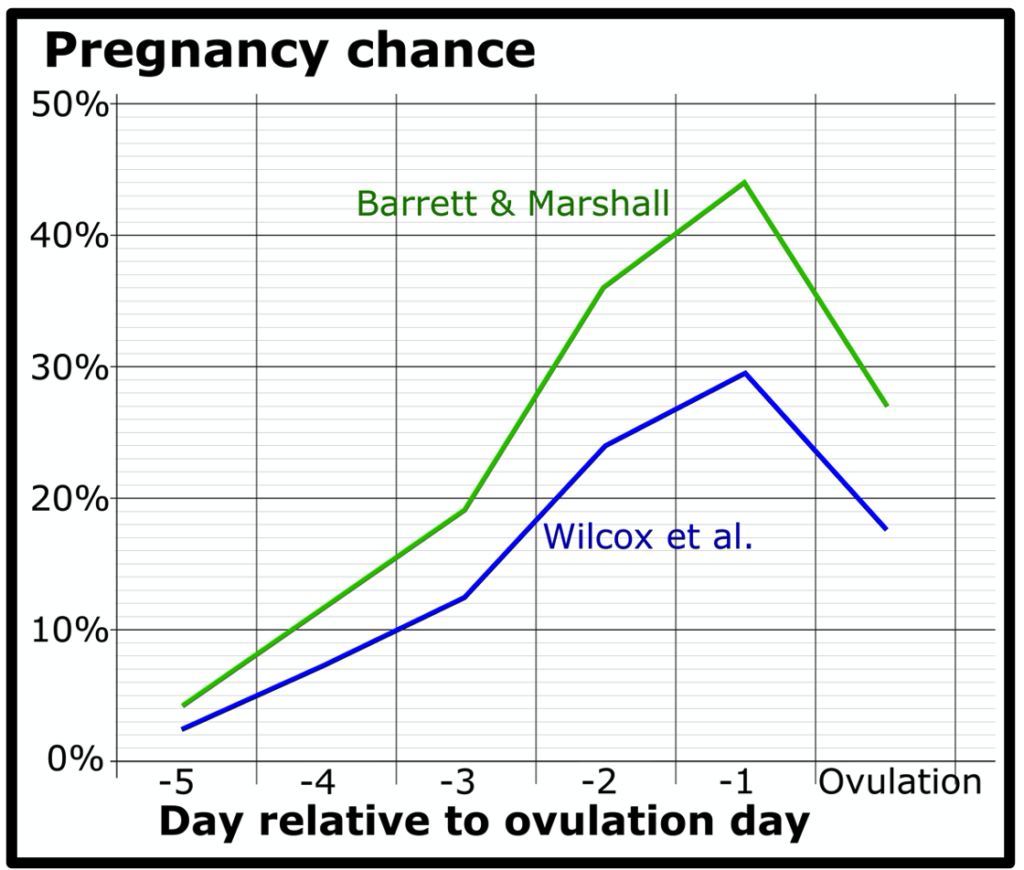
Fertility awareness-based methods—Understanding the monthly fertility pattern of a person who menstruates can help with planning to get pregnant or avoid getting pregnant. The fertility pattern is the number of days in the month when a person is fertile (able to get pregnant), the days when infertile, and days when fertility is unlikely, but possible. People who have a regular menstrual cycle generally have nine or more fertile days each month. Those wishing not to become pregnant should avoid intercourse on these days, or a barrier method should be used. Failure rates vary across these methods. Range of typical use failure rates: 2-23
Lactational Amenorrhea Method
For people who have recently had a baby and are breastfeeding, the Lactational Amenorrhea Method (LAM) can be used as birth control when three conditions are met:
- Amenorrhea (not having any menstrual periods after delivering a baby)
- Fully or nearly fully breastfeeding (no interval greater than 6 hours between feedings)
- Less than 6 months after delivering a baby.
LAM is a temporary and relatively unreliable method of birth control, and another birth control method must be used when any of the three conditions are not met. Failure rate of ~2% within 6 months of giving birth.
Emergency Contraception
Emergency contraception is not a regular method of birth control. Emergency contraception can be used after no birth control was used during sex, or if the birth control method failed, such as if a condom broke.
- Copper IUD—A copper T IUD may be inserted into the uterus within five days of unprotected sex.
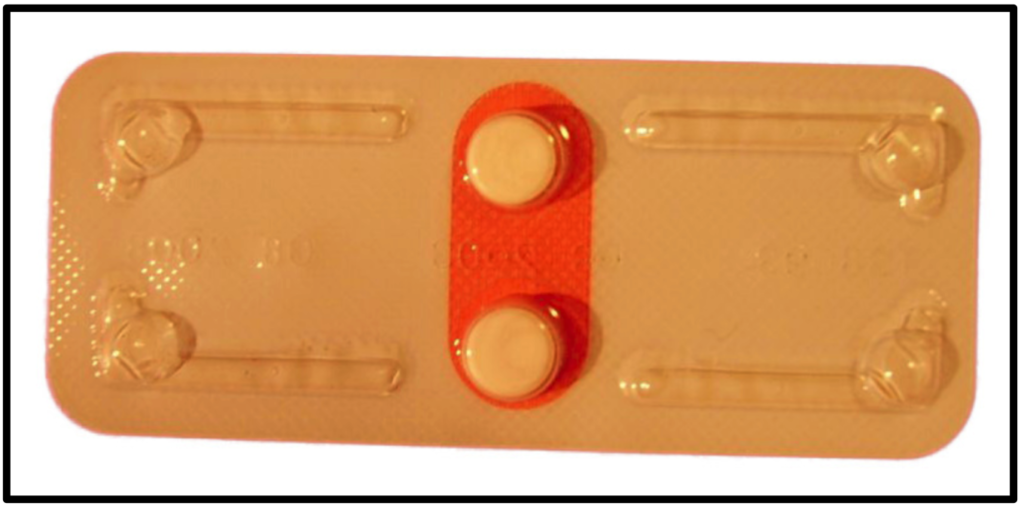
- Emergency contraceptive pills—People with a uterus and ovaries can take emergency contraceptive pills up to 5 days after unprotected sex, but the sooner the pills are taken, the better they will work. There are three different types of emergency contraceptive pills available in the United States. Some emergency contraceptive pills are available over the counter.
Permanent Methods of Birth Control
- Tubal ligation or “tying tubes”— A person with ovaries can have the fallopian tubes tied (or closed) so that sperm and eggs cannot meet for fertilization. The procedure can be done in a hospital or in an outpatient surgical center. This method is effective immediately. Typical use failure rate: 0.5%.
- Vasectomy—This operation is done to keep sperm from going to the penis, so ejaculate will contain no sperm that could fertilize an egg. The procedure is typically done at an outpatient surgical center. About 12 weeks after the operation, a doctor should verify that the sperm count has dropped to zero. Another form of birth control should be used until the man’s sperm count has dropped to zero. Typical use failure rate: 0.15%.
Text from Centers for Disease Control and Prevention: https://www.cdc.gov/reproductivehealth/contraception/index.htm
To complete this activity, answer the questions in the worksheet, and fill in the table (pictured below; it is fillable in the worksheet).
| Method | Category | Description | Typical Failure Rate |
|---|---|---|---|
| IUD | Intrauterine | Small “T”-shaped device that is placed in the uterus | |
| Implant | Thin rod containing progestin inserted under the skin of the arm | 0.01% | |
| Injection | Hormonal | 4.0% | |
| Hormonal | Pills taken daily that contain the hormones estrogen and progestin | 7.0% | |
| Diaphragm | Barrier | 17% | |
| Condom | Latex sheath worn over a penis | ||
| Barrier | Foam, gel, cream, film, suppository or tablet that kills sperm | ||
| Emergency | Pills that can be taken by a person with a uterus up to 5 days after intercourse | N/A | |
| Vasectomy | Surgery performed to prevent sperm from traveling to the penis | ||
| Chemical | Vaginal gel inserted before intercourse that alters vaginal pH to lower the mobility of sperm | 14.0% | |
| N/A | 0% |
Navigation
Introduction: https://wendystjohn.summerlark.net/2021/10/01/110-human-reproduction/
Life’s Greatest Miracle: https://wendystjohn.summerlark.net/2021/10/01/lifes-greatest-miracle/
Fetal Alcohol Syndrome: https://wendystjohn.summerlark.net/2021/03/10/fetal-alcohol-syndrome/
Sexually Transmitted Diseases: https://wendystjohn.summerlark.net/2021/01/28/sexually-transmitted-diseases/
Contraception: https://wendystjohn.summerlark.net/2020/10/12/contraception/