Introduction
Sexual reproduction was an early evolutionary innovation after the appearance of eukaryotic cells. It appears to have been very successful because most eukaryotes are able to reproduce sexually, and in many animals, it is the only mode of reproduction. And yet, scientists recognize some real disadvantages to sexual reproduction.
On the surface, creating offspring that are genetic clones of the parent appears to be a better system. If the parent organism is successfully occupying a habitat, offspring with the same traits would be similarly successful. There is also the obvious benefit to an organism that can produce offspring whenever circumstances are favorable by asexual budding, fragmentation, or asexual eggs. These methods of reproduction do not require another organism of the opposite sex. Indeed, some organisms that lead a solitary lifestyle have retained the ability to reproduce asexually. In addition, in asexual populations, every individual is capable of reproduction. In sexual populations, the males are not producing the offspring themselves, so in theory an asexual population could grow twice as fast.
However, multicellular organisms that exclusively depend on asexual reproduction are exceedingly rare. Why is sexuality (and meiosis) so common? This is one of the important questions in biology and has been the focus of much research beginning in the latter half of the twentieth century. There are several possible explanations, one of which is that the variation that sexual reproduction creates among offspring is very important to the survival and reproduction of the population. Thus, on average, a sexually reproducing population will leave more descendants than an otherwise similar asexually reproducing population. The only source of variation in asexual organisms is mutation. This is the ultimate source of variation in sexual organisms, but in addition, those different mutations are continually reshuffled from one generation to the next when different parents combine their unique genomes and the genes are mixed into different combinations by crossovers during prophase I and random assortment at metaphase I.
Gestation
Gestation refers to the developmental period that takes place while an embryo is developing in the womb. Also called pregnancy, in humans this period takes approximately 40 weeks, although it can last anywhere between 36 and 42 weeks after fertilization and still be considered within the “normal” timeframe. We break this gestational period down further into three trimesters, to more easily categorize the developmental stages that happen throughout the process.
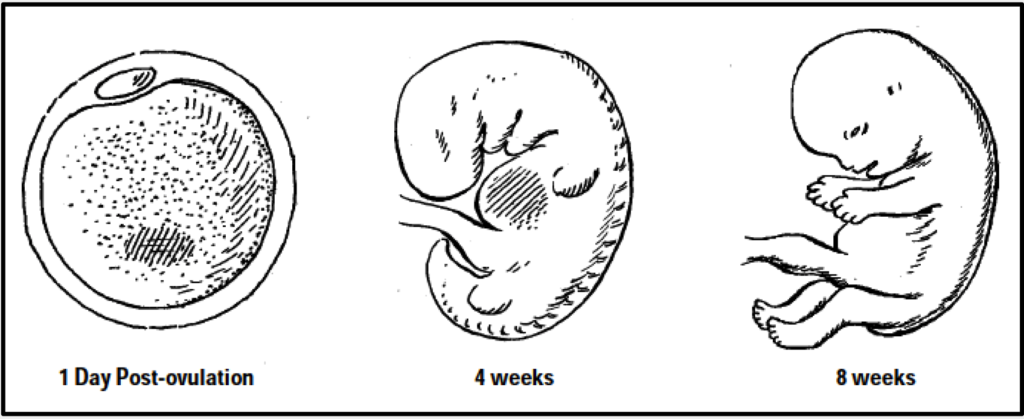
First Trimester: An egg becomes fertilized when a sperm penetrates it, creating a zygote. Embryonic development begins with simple cell division and proceeds through cell differentiation, morphogenesis (formation of body structures), and growth. For the first eight weeks, the developing baby is called an embryo, and looks like a tadpole. At about three weeks, the neural tube, which becomes the brain and spinal cord, is forming. At about four weeks, the heart begins to pump blood. Tiny limb buds appear, ankles and wrists are formed, and fingers and toes develop. During the first trimester, which lasts up to 10 weeks, all major body organs and systems are formed but not completely developed. This is a critical period for development of the heart, central nervous system, upper and lower limbs, eyes and ears, teeth and palate, and most organs. Any damage at this stage can result in major damage or deformity. At eight weeks, when most organs have formed, the embryo is called a fetus.
Second Trimester: The fetus moves, kicks, swallows, and can hear the mother’s voice. It begins to wake and sleep at regular intervals. The skin changes from a transparent pink to a wrinkled red, and is covered with soft, fine hair. By the end of the fourth month, the central nervous system is past its most vulnerable stage. As its development continues, though, it remains susceptible to functional defects throughout pregnancy. The eyes, teeth, and external genitalia continue to be susceptible to functional defects and lesser deformities throughout the second trimester, which lasts until about Week 30.
Third Trimester: Body growth slows down, while brain growth continues and the head grows larger during the third trimester. The fetus begins developing its own immune system. Rapid brain growth continues. The fetus can open and close its eyes, suck its thumb, kick, stretch, and cry. It responds to light and sound and, if born as early as the seventh month, would have a good chance of surviving.
Text adapted from materials that accompany the NOVA Activity: “Life’s Greatest Miracle”
Life’s Greatest Miracle
Access the worksheet at the link below, and make a copy to your own Google Drive. (You will not be able to edit the original liked file). After you complete the worksheet, download it as a PDF file and email to your lab instructor with “110 Make-up Lab” in the subject line.
https://www.pbs.org/wgbh/nova/video/lifes-greatest-miracle/

- What percentage of multi-cellular organisms on Earth use sexual reproduction?
- How fast is sperm produced in a male?
- Why is the increase in genetic diversity considered advantageous in humans or any species?
- When does egg production begin in a female?
- What is the protein shell that surrounds the egg called?
- How does the sperm gain access to the egg once it encounters the protein shell that surrounds the egg?
- How would you characterize a blastocyst (also known as a blastula)?
- What is the process called when the cells organize themselves into an embryo (i.e. they form three distinct types of tissue or germ layers)?
- What gene is contained on the Y chromosome that codes for “maleness”? And what hormone does it causes the gonads to produce that generates male structures?
- Why is human birth considered to be more dangerous than many mammals species, and other primate species?
Follow up questions:
- When the sex cells made copies of the chromosomes before they divided, in which phase of the cell cycle did the copying (replication) take place?
- When chromosomes pair up next to each other and trade parts of the chromosomes with their partners:
- Scientists call these pairs of chromosomes:
- The process when the chromosomes within a pair exchange parts is known as:
- In which phase of the cell cycle does this all happen?
- How many sperm cells are produced from one sex cell in males? What is the key difference between these cells and other cells in the body?
- When the sperm reaches the egg and one sperm is able to penetrate the zona the get to the egg surface. Describe the series of reactions that must occur to allow that sperm in.
- Once a single sperm triggers the egg to begin the fertilization process, how does the egg prevent polyspermy?
- Once the developing blastula undergoes gastrulation, name the three germ layers that are formed and identify what sorts of structures are formed from each germ layer.
Birth Control Methods
Many people who have a uterus and ovaries can potentially become pregnant. People with a penis and testes are potentially capable of getting someone pregnant. For people who are sexually active yet wish to avoid pregnancy, many elements need to be considered when choosing the most appropriate contraceptive method. These elements include safety, effectiveness, availability (including accessibility and affordability), and preference. Voluntary informed choice of contraceptive methods is essential, and contraceptive counseling, when applicable, might be an important contributor to the successful use of contraceptive methods.
In choosing a method of contraception, dual protection from the simultaneous risk for HIV and other STDs also should be considered. Although hormonal contraceptives and IUDs are highly effective at preventing pregnancy, they do not protect against STDs, including HIV (the virus that causes AIDS). Consistent and correct use of latex condoms reduces the risk for HIV infection and other STDs, including chlamydial infection, gonococcal infection, and trichomoniasis.
Ultimately, though, when it comes to heterosexual sex between a partner with a uterus and a partner who produces sperm, the only 100% guaranteed way to avoid pregnancy is abstinence (refraining from sexual activity). For sexually active people of any orientation, wearing condoms may reduce the risk of STDs.
Reversible Methods of Birth Control

Intrauterine Contraception
- Copper T intrauterine device (IUD) —This IUD is a small device that is shaped in the form of a “T.” A doctor places it inside the uterus to prevent pregnancy. It can stay in the uterus for up to 10 years. Typical use failure rate: 0.8%.
- Levonorgestrel intrauterine system (LNG IUD)—The LNG IUD is a small T-shaped device like the Copper T IUD. It is also placed inside the uterus by a doctor. It releases a small amount of progestin each day to prevent pregnancy. The LNG IUD stays in the uterus for up to 5 years. Typical use failure rate: 0.1-0.4%.
Hormonal Methods (for use by people with a uterus and ovaries)

- Implant—The implant is a single, thin rod that is inserted under the skin of the upper arm. The rod contains a progestin that is released into the body over 3 years. Typical use failure rate: 0.01%
- Injection or “shot” (e.g. Depo-provera) —A shot of the hormone progestin in the buttocks or arm every three months. Typical use failure rate: 4%.
- Combined oral contraceptives—Also called “the pill,” combined oral contraceptives contain the hormones estrogen and progestin, and are prescribed by a doctor. A pill is taken at the same time each day. Doctors may advise people older than 35 years who smoke, or have a history of blood clots or breast cancer, to not use the pill. Typical use failure rate: 7%.
- Progestin only pill—Unlike the combined pill, the progestin-only pill (sometimes called the mini-pill) only has one hormone, progestin, instead of both estrogen and progestin, and is prescribed by a doctor. It is taken at the same time each day and may be a good option for people who can’t take estrogen. Typical use failure rate: 7%.
- Patch—This skin patch is worn on the lower abdomen, buttocks, or upper body (but not on the breasts). Prescribed by a doctor, this method releases hormones progestin and estrogen into the bloodstream. A new patch is applied once a week for three weeks. During the fourth week, no patch is worn, to allow for a menstrual period. Typical use failure rate: 7%.
- Hormonal vaginal contraceptive ring—The ring releases progestin and estrogen. You place the ring inside your vagina. You wear the ring for three weeks, take it out for the week you have your period, and then put in a new ring. Typical use failure rate: 7%.
Chemical Methods
- Spermicides—These products work by killing sperm and come in several forms—foam, gel, cream, film, suppository, or tablet. They are placed in the vagina no more than one hour before intercourse. They are then left in place at least six to eight hours after intercourse. A spermicide may be used in addition to a male condom, diaphragm, or cervical cap. They can be purchased at drug stores. Typical use failure rate: 21%.
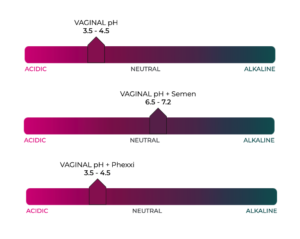
- Phexxi: This on-demand vaginal gel is relatively new, and acts by altering vaginal pH to reduce the motility of sperm, making them unable to swim up the vaginal canal to fertilize an egg. Typical use failure rate: 14% (7% when used as directed).

Barrier Methods
- Diaphragm or cervical cap—These are placed inside the vagina to cover the cervix to block sperm. The diaphragm is shaped like a shallow cup. The cervical cap is a thimble-shaped cup. Before sexual intercourse, one or the other would be inserted, along with spermicide, to block and/or kill sperm. They come in different sizes, so a doctor should be consulted for proper fit. Typical use failure rate for the diaphragm: 17%.
- Sponge—The contraceptive sponge contains spermicide and is placed in the vagina where it fits over the cervix. The sponge works for up to 24 hours and must be left in the vagina for at least 6 hours after the last act of intercourse, at which time it is removed and discarded. Typical use failure rate: 14% for people who have never given birth and 27% for those who have had a baby.

- “Male” condom—Worn on the penis, the condom keeps sperm from getting into the partner’s body. Latex condoms, the most common type, help prevent pregnancy, and HIV and other STDs, as do the newer synthetic condoms. “Natural” or “lambskin” condoms also help prevent pregnancy, but may not provide protection against STDs, including HIV. Typical use failure rate: 13%. Condoms can only be used once. They can be purchased, along with KY jelly, or water-based lubricants, at a drug store. Do not use oil-based lubricants such as massage oils, baby oil, lotions, or petroleum jelly with latex condoms. They will weaken the condom, causing it to tear or break.
- “Female” condom—Worn inside the vagina, this device helps prevent sperm from getting into the body. It is packaged with a lubricant and is available at drug stores. It can be inserted up to eight hours before sexual intercourse. Typical use failure rate: 21%, and also may help prevent STDs. Should not be used in conjunction with a “male” condom, as this could cause one or the other barrier to tear.
- Dental dams – latex or polyurethane sheets used between the mouth and vagina or anus during oral sex. While dental dams do not aid in contraception, they can act as protection against sexually transmitted pathogens.
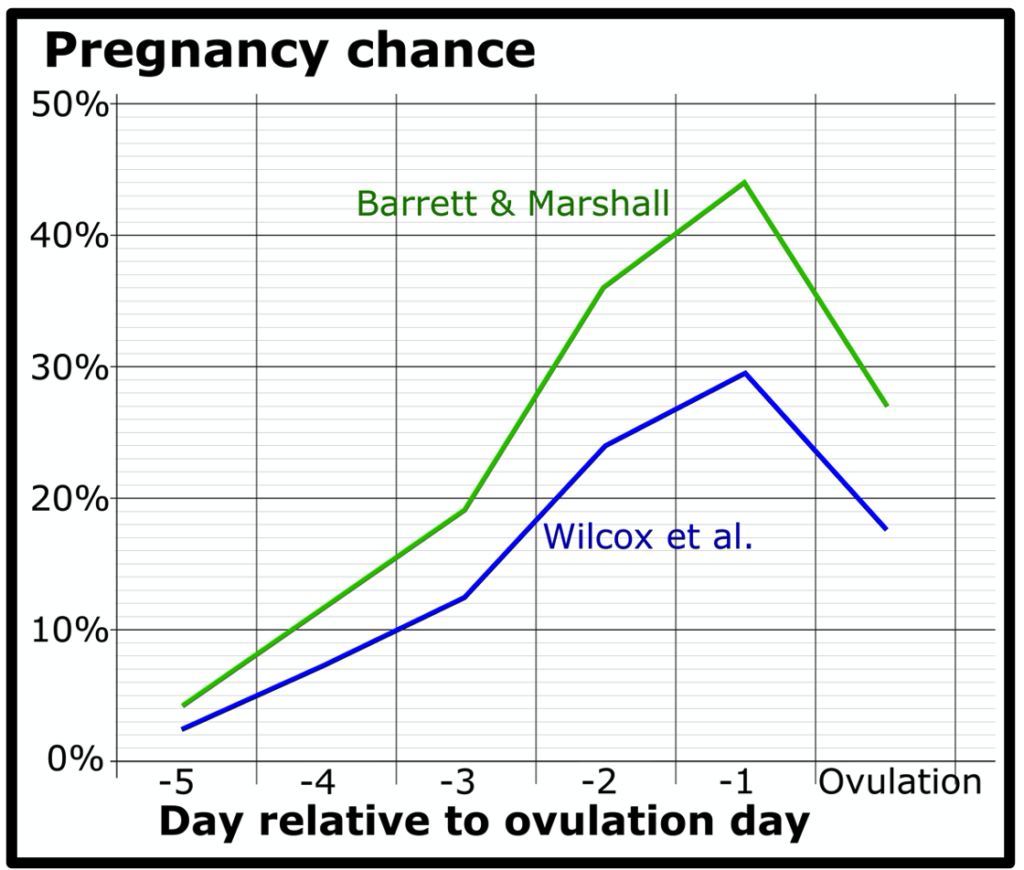
Fertility Awareness-Based Methods
Fertility awareness-based methods—Understanding the monthly fertility pattern of a person who menstruates can help with planning to get pregnant or avoid getting pregnant. The fertility pattern is the number of days in the month when a person is fertile (able to get pregnant), the days when infertile, and days when fertility is unlikely, but possible. People who have a regular menstrual cycle generally have nine or more fertile days each month. Those wishing not to become pregnant should avoid intercourse on these days, or a barrier method should be used. Failure rates vary across these methods. Range of typical use failure rates: 2-23
Lactational Amenorrhea Method
For people who have recently had a baby and are breastfeeding, the Lactational Amenorrhea Method (LAM) can be used as birth control when three conditions are met:
- Amenorrhea (not having any menstrual periods after delivering a baby)
- Fully or nearly fully breastfeeding (no interval greater than 6 hours between feedings)
- Less than 6 months after delivering a baby.
LAM is a temporary and relatively unreliable method of birth control, and another birth control method must be used when any of the three conditions are not met. Failure rate of ~2% within 6 months of giving birth.
Emergency Contraception
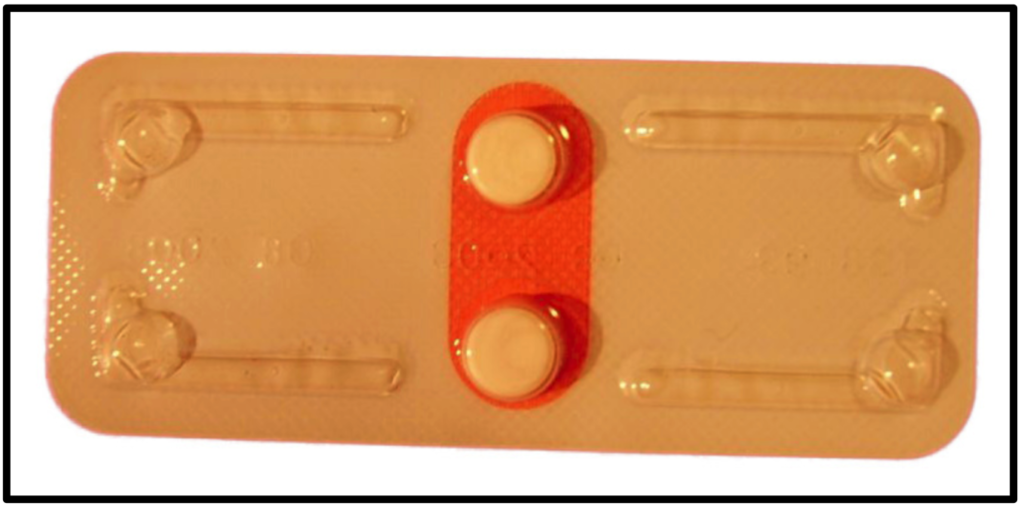
Emergency contraception is not a regular method of birth control. Emergency contraception can be used after no birth control was used during sex, or if the birth control method failed, such as if a condom broke.
- Copper IUD—A copper T IUD may be inserted into the uterus within five days of unprotected sex.
- Emergency contraceptive pills—People with a uterus and ovaries can take emergency contraceptive pills up to 5 days after unprotected sex, but the sooner the pills are taken, the better they will work. There are three different types of emergency contraceptive pills available in the United States. Some emergency contraceptive pills are available over the counter.
Permanent Methods of Birth Control
- Tubal ligation or “tying tubes”— A person with ovaries can have the fallopian tubes tied (or closed) so that sperm and eggs cannot meet for fertilization. The procedure can be done in a hospital or in an outpatient surgical center. This method is effective immediately. Typical use failure rate: 0.5%.
- Vasectomy—This operation is done to keep sperm from going to the penis, so ejaculate will contain no sperm that could fertilize an egg. The procedure is typically done at an outpatient surgical center. About 12 weeks after the operation, a doctor should verify that the sperm count has dropped to zero. Another form of birth control should be used until the man’s sperm count has dropped to zero. Typical use failure rate: 0.15%.
Text from Centers for Disease Control and Prevention: https://www.cdc.gov/reproductivehealth/contraception/index.htm
To complete this activity, answer the questions below, then print out and fill in the table :
- Which reversible method of birth control listed below is most effective against pregnancy?
- Male” condoms
- Copper IUD
- Oral contraceptives
- Spermicide
- Implant
- Which reversible method of birth control listed below is most effective against STDs?“
- Male” condoms
- Copper IUD
- Oral contraceptives
- Spermicide
- Implant
- Given that the answers to the two questions above are different, what would you suggest as being the best method of protection against BOTH pregnancy and STDs?
- What type of lubricants should NOT be used with latex condoms, as they can cause them to tear or break? (select all that apply)
- KY jelly
- Water-based lubricants
- Baby oil
- Petroleum jelly
- LAM is a method that may be effective under what circumstances?
- When partners are only engaging in oral sex
- For a few months after giving birth to a child
- When the pill is taken within 5 days of unprotected sexual activity
- When hormone shots are given regularly, at three-month intervals
- The fertility awareness method involves . . .
- “Pulling out” of the vagina before ejaculation
- Having a surgical procedure to prevent the possibility of fertility
- Insertion of a T-shaped device into the uterus
- Keeping track of the menstrual cycle, to avoid having sex during the fertile period
- Overall, are hormonal methods or barrier methods of contraceptives more effective against pregnancy?
- Which birth control method is 100% effective?
- The Pill.
- Diaphram.
- Abstinence.
- Condoms.
| Method | Category | Description | Typical Failure Rate |
|---|---|---|---|
| IUD | Intrauterine | Small “T”-shaped device that is placed in the uterus | |
| Implant | Thin rod containing progestin inserted under the skin of the arm | 0.01% | |
| Injection | Hormonal | 4.0% | |
| Hormonal | Pills taken daily that contain the hormones estrogen and progestin | 7.0% | |
| Diaphragm | Barrier | 17% | |
| Condom | Latex sheath worn over a penis | ||
| Barrier | Foam, gel, cream, film, suppository or tablet that kills sperm | ||
| Emergency | Pills that can be taken by a person with a uterus up to 5 days after intercourse | N/A | |
| Vasectomy | Surgery performed to prevent sperm from traveling to the penis | ||
| Chemical | Vaginal gel inserted before intercourse that alters vaginal pH to lower the mobility of sperm | 14.0% | |
| N/A | 0% |